Spinal Cord Stimulation (SCS) : An Innovative Solution for Sustainable Relief from Chronic Pain

Spinal Cord Stimulation (SCS): An Innovative Solution for Sustainable Chronic Pain Management
When Conventional Treatments Are No Longer Enough Technology Can Help
Many patients continue to suffer from chronic painsuch as back pain, leg pain, numbness, burning sensations, or neuropathic paineven after receiving medications, physical therapy, or surgery.
Spinal Cord Stimulation (SCS) has been recognized worldwide as an effective treatment option for managing chronic pain in patients who do not respond to traditional therapies.
What Is Spinal Cord Stimulation (SCS)?
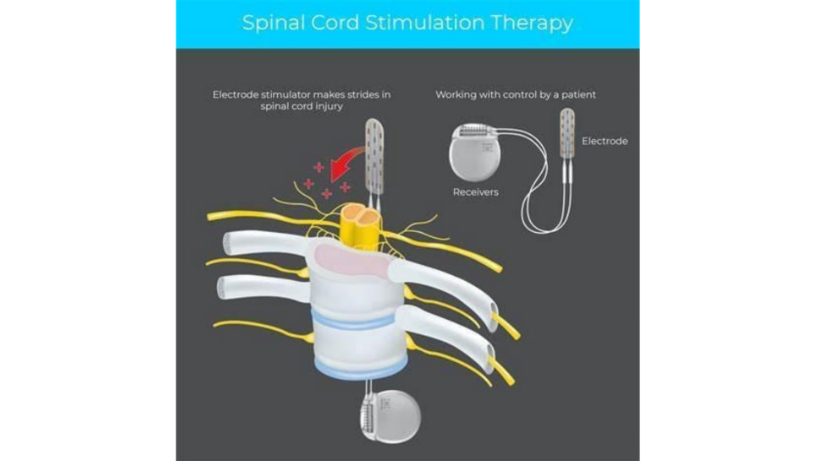
Spinal Cord Stimulation (SCS) is an advanced technology that delivers mild electrical impulses to the spinal cord through implanted electrodes.
These electrical signals alter the way the brain perceives pain, resulting in reduced pain sensations.
SCS helps decrease dependence on pain medication and enables patients to return to daily activities with improved comfort and mobility.
Who Is a Candidate for SCS?
SCS may benefit patients with:
- Failed Back Surgery Syndrome (FBSS): Persistent pain after spinal surgery
- Complex Regional Pain Syndrome (CRPS): Chronic pain with swelling, redness, or hypersensitivity
- Peripheral Neuropathy: Chronic nerve pain causing numbness or burning sensations in hands or feet
- Ischemic Limb Pain: Pain due to poor blood circulation in the arms or legs
Note: Eligibility for SCS depends on evaluation by a pain management specialist.
Treatment Phases: Trial and Permanent Implantation
1. Trial Phase
- A temporary electrode is inserted into the spinal canal using a needle under X-ray guidance.
- The electrode is connected to an external stimulator,
- allowing patients to test the device for about 5-7 days.
During this time, patients record their pain levels, activities, and sleep quality.
If pain relief exceeds > 50% and quality of life improves, the patient may proceed to the next phase.
Once successful during the trial, a minor surgery is performed to implant the permanent device.
- Electrodes and a small battery are implanted under the skin (usually near the hip or abdomen).
- Patients can control stimulation levels using a remote device.
- Regular follow-up visits ensure optimal adjustment of the settings.
- After surgery, patients should temporarily avoid heavy lifting, twisting, or bending to prevent electrode displacement.

- Some patients describe a mild tingling or gentle electrical sensation (called paresthesia) at the pain site.
- Modern devices can provide effective pain relief without this sensation.
- Perception may vary with body position changes, such as sitting or standing.
- Significant reduction in chronic pain
- Decreased reliance on long-term pain medication
- Improved mobility and daily function
- Enhanced sleep quality and emotional well-being
- High safety profile under specialist supervision
- Electrode lead displacement
- Infection at the implantation site
- Cerebrospinal fluid (CSF) leakage
- Electrical shock or unintended stimulation
- Some patients may not respond to stimulation in the long term
Battery Types
| Type | Lifespan | Advantages | Considerations |
| Rechargeable | 8 - 10 years | No frequent replacement Requires | regular charging |
| Non-rechargeable | 25 years | No charging required | Needs surgical replacement when depleted |
Living with an SCS Device
You Can:
- Perform daily activities walk, drive, shower, use phones and microwaves
- Carry your device ID card when traveling or receiving medical treatment
- MRI: Only with compatible models; always inform medical staff
- Electrocautery: Turn off SCS before use during procedures
- Diathermy: Strictly prohibited may damage the device
- Physical therapy: avoid forceful spinal manipulation, deep ultrasound, and electrical stimulation near the SCS.
- For any future surgeries, always inform your doctor that you have an implanted SCS.
- Surgery or Airports: Inform staff and show your device ID; turn off the system before entering magnetic fields
If SCS is not suitable, other options include:
- Medication management (oral, injectable, or patch)
- Physical therapy
- Nerve block injections
- Spinal surgery (for structural abnormalities)
SCS remains a key treatment for patients who have not found relief from other modalities.
Why Choose SCS at Sapiens Pain Hospital

At Sapiens Pain Hospital, we provide personalized pain management through advanced medical technology and holistic care.
Our Strengths:
- Multidisciplinary team of specialists in Pain Medicine, Neurosurgery, and Rehabilitation Medicine
- Comprehensive care pathway from screening and trial to implantation and long-term follow-up
- Post-treatment rehabilitation programs supported by physical therapists and clinical psychologists
- On-site and telehealth consultations for local and international patients
- International-level medical standards and patient safety
Contact Us
Sapiens Pain Hospital The Specialized Center for Pain Management
Prachapattana Road (next to SISB International School)
Tel: 02-111-3703
Website: www.sapienspainhospital.com
Open daily with dedicated specialists ready to care for you.
Reference
1. Deer, T. R., et al. (2014). The appropriate use of neurostimulation of the spinal cord and peripheral nervous system for the treatment of chronic pain and ischemic diseases: The Neuromodulation Appropriateness Consensus Committee. Neuromodulation: Technology at the Neural Interface, 17(6), 515550.
2. Kumar, K., et al. (2007). Spinal cord stimulation is effective in the management of failed back surgery syndrome: Long-term clinical outcome study. Neurosurgery, 60(5), 884893.
3. Mekhail, N., et al. (2020). Cost-effectiveness of spinal cord stimulation for chronic pain management: a systematic review. Clinical Journal of Pain, 36(6), 429436.
4. North, R. B., et. al. (2005). Spinal cord stimulation versus reoperation for failed back surgery syndrome: a cost effectiveness and cost utility analysis based on a randomized, controlled trial. Neurosurgery, 56(5), 10811088.
5. International Neuromodulation Society. What is Spinal Cord Stimulation (SCS)?
6. Medtronic. (2023). Living with Spinal Cord Stimulation.
7. Neuromodec. SCS Patient Guide: MRI, Diathermy, and Cautions.


